Giving Aged Care facilities clarity during Australia’s largest funding reform
Supporting 60,000+ residential aged-care beds through the national shift to AN-ACC.
The challenge facing aged-care facilities
Overview
In response to the Royal Commission, the Australian Government replaced ACFI with AN-ACC, a new funding model for residential aged care. This shift required providers to adapt quickly so they could understand funding outcomes, gather accurate evidence, and reduce compliance risk during the transition.
Clinical Manager, Telstra Health’s aged-care platform, is used across 60,000+ residential beds. Its existing ACFI workflows could not support the AN-ACC model. Staff urgently needed clarity, predictable workflows, and confidence ahead of government assessments.
I led the UX work to design a new assessment experience aligned with AN-ACC structure, guided by real user insight and shaped around the needs of clerical and nursing staff.
Problem
Aged Care facilities needed a reliable, structured way to understand AN-ACC funding outcomes and collect evidence that would withstand audits and assessor reviews. The existing ACFI workflow did not map to AN-ACC, and attempting to retrofit it would introduce risk, confusion, and errors.
Key challenges:
High staff anxiety around funding loss
Fear that government assessors could misinterpret resident needs
Difficulty finding and linking evidence across multiple parts of the system
Unclear terminology and inconsistent UI patterns
No way to preview or validate AN-ACC outcomes
Legacy interface with high cognitive load
Facilities needed a clear, linear workflow that made evidence capture easy, transparent, and tied to each part of the assessment.
Funding reform and design implications
From ACFI to AN-ACC
The move from ACFI to AN-ACC changed how funding is calculated and who controls the assessment process.
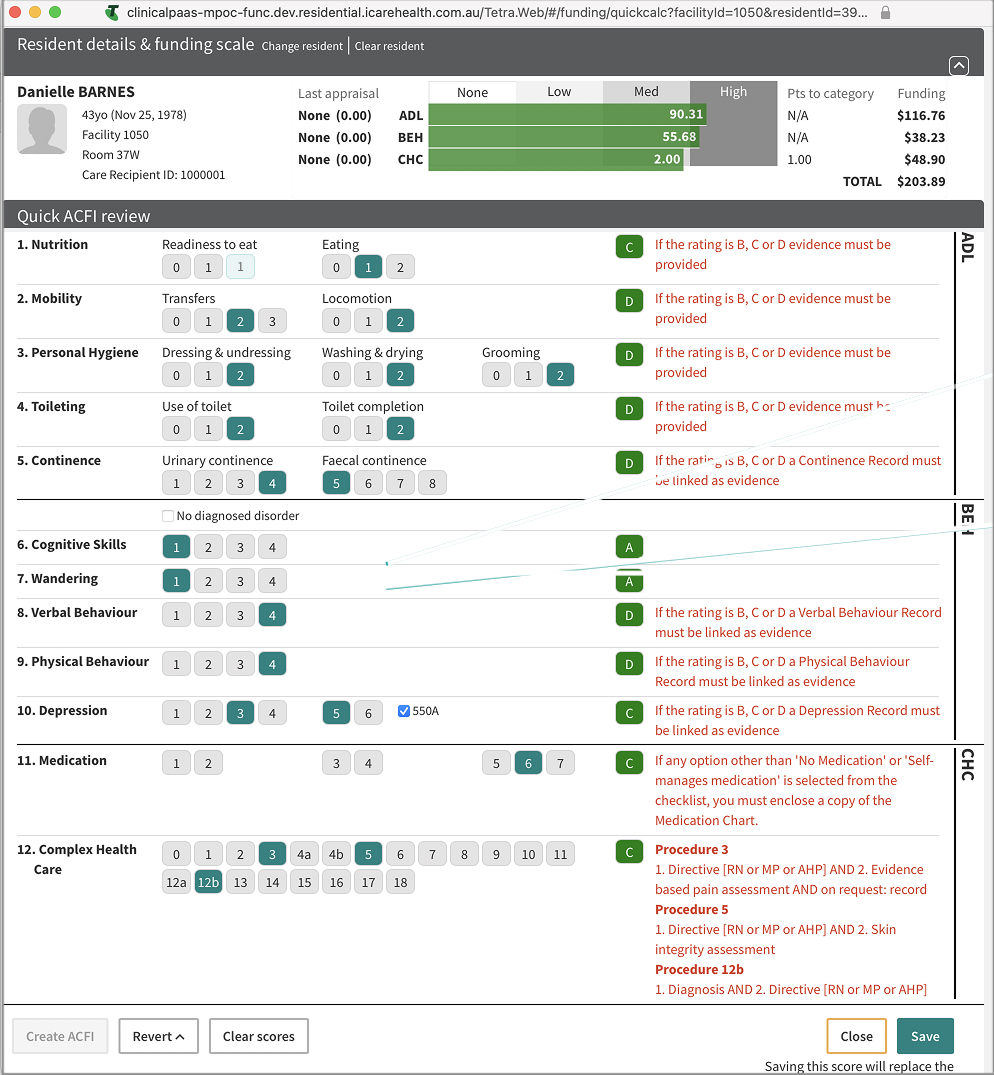
Under ACFI:
Facilities completed their own assessments
Internal “quick calculators” helped estimate funding
Some providers focused on “resident shopping” to optimise revenue
Evidence was often scattered across documents and notes
Under AN-ACC:
Independent government assessors complete the classification
Funding is tied to a standardised national assessment tool
Evidence must be clear, traceable, and defensible
Providers have less control and higher anxiety about outcomes
For providers, the reform was not only a new formula. It was a loss of perceived control and a higher bar for documentation and transparency.
After analysing both models and walking through the current ACFI workflow, I found that:
AN-ACC domains do not map cleanly to ACFI
Scoring logic is different
Evidence expectations are more structured
Retrofitting would increase complexity rather than reduce it
Based on this analysis, a targeted redesign became the clearer, safer option.
The change from ACFI to AN-ACC
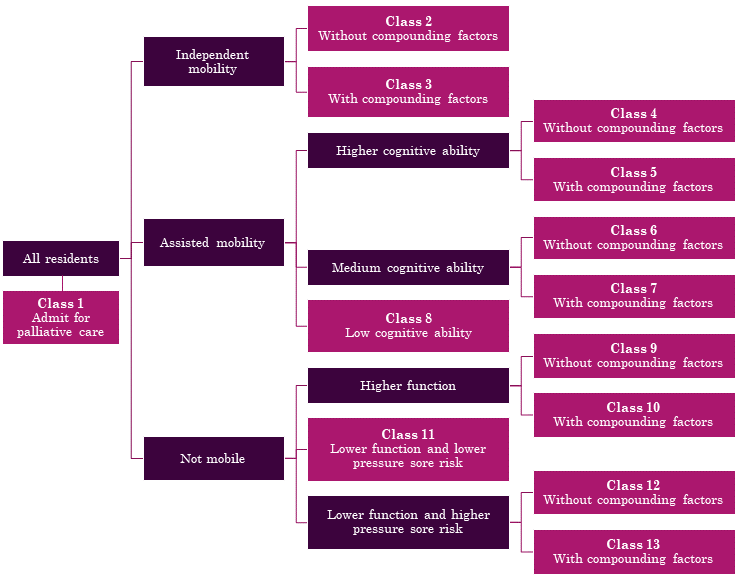
AN-ACC Classifications
Before recommending a redesign, I explored whether the existing ACFI workflow could be adapted for AN-ACC. Reuse would have been faster to deliver, easier for development, and less disruptive for staff.
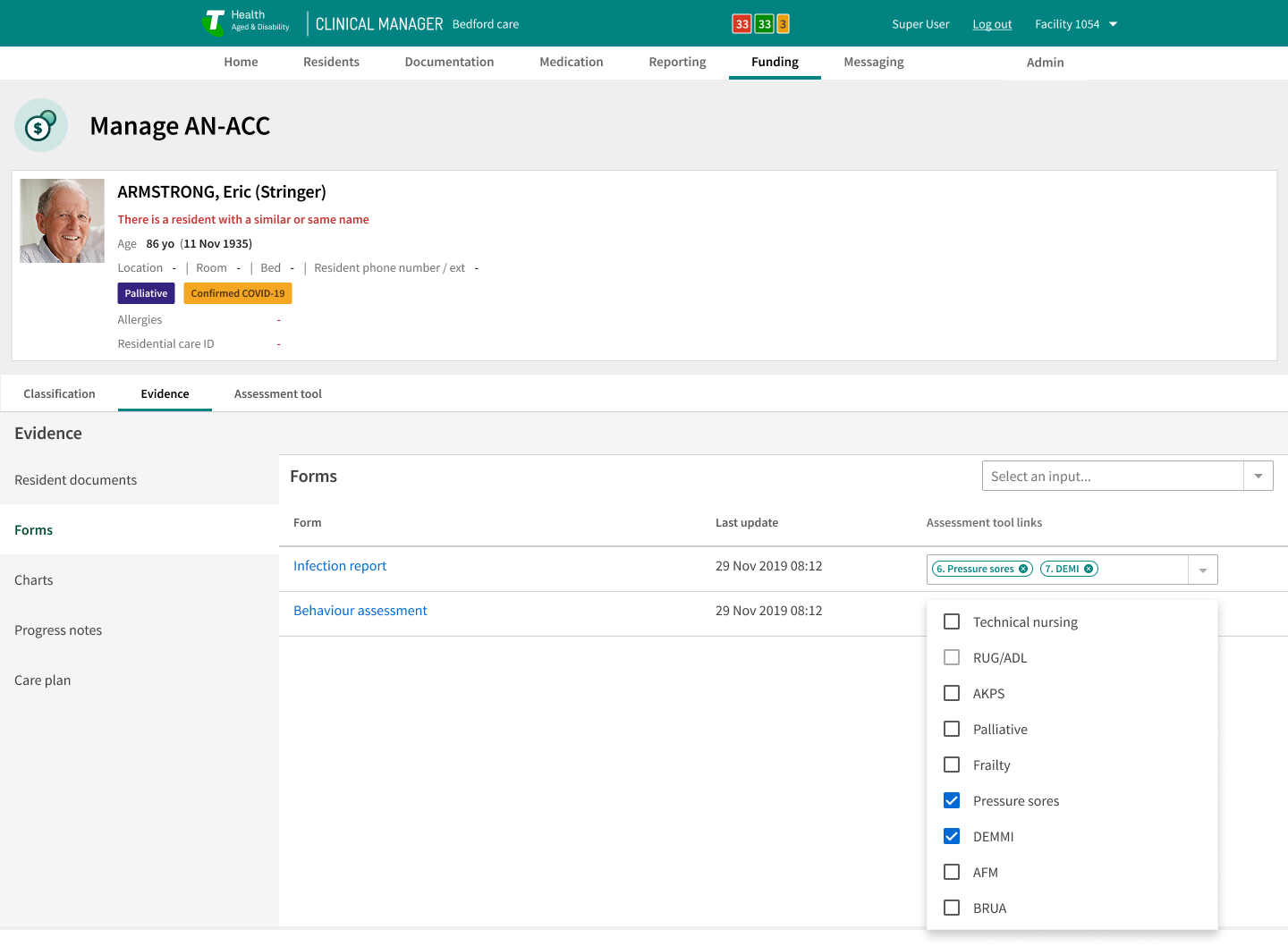
AN-ACC Assessment Criteria
Technical Nursing Requirements
Resource Utilisation Groups & Activities of Daily Living (RUG-ADL)
Australia-modified Karnofsky Performance Status (AKPS)
Palliative Care
Frailty
Braden Scale for Predicting Pressure Sore Risk
De Moreton Mobility Index (DEMMI) - Modified
Australian Functional Measure (AFM)
Behaviour Resource Utilisation Assessment (BRUA)
Old ACFI funding calculator
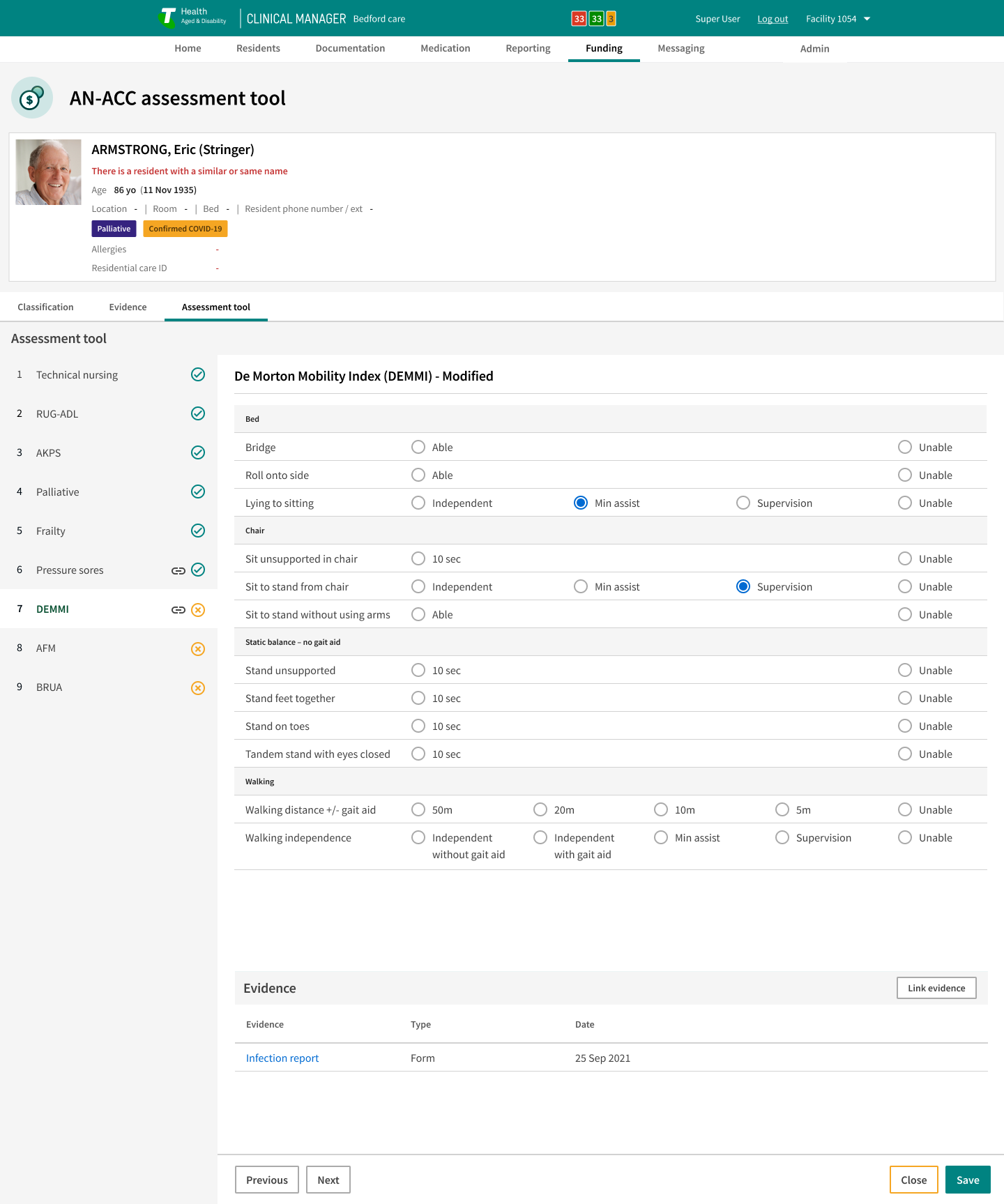
What this meant for Clinical Manager
These changes created specific requirements for Clinical Manager and for the UX:
Staff needed a way to understand likely AN-ACC outcomes before an assessor visit
Evidence had to be easy to find and link to assessment items
The system needed to reduce anxiety by showing a clear, stepwise process
Old ACFI workflows and calculators could not simply be repurposed
The design had to support both day-to-day documentation and funding preparation
The UX response focused on building a resident-centred assessment flow that aligned with the AN-ACC tool, while giving facilities better visibility of their evidence and funding risk.
Can we adapt current workflows?
What staff needed to feel supported
Research and insights
I interviewed clerical staff from five residential aged-care facilities. Their concerns were consistent and shaped the redesign:
Anxiety about misclassification and revenue loss
Confusion around new AN-ACC requirements
Difficulty finding clinical evidence in the existing system
Desire for predictable, linear assessment sequences
Need for terminology that reflected real practice
Key insights:
Evidence must be accessible in context
The assessment must flow in a clear, expected sequence
Terminology must match the language used on the floor
Layout must reduce cognitive load
Repurposing ACFI screens would create risk and confusion
Synthesised insights across 4 facilities.
Design strategy
The strategy centred on creating a safe, predictable assessment experience within a legacy system:
Align the user flow directly with AN-ACC’s structure
Build evidence-tagging into each step of the workflow
Use consistent layout patterns to reduce cognitive load
Validate direction with clerical users through iterative testing
Work closely with BAs to interpret government scoring logic
Deliver incrementally to fit within the legacy technical constraints
Design decisions & iterations
Key decisions
A structured assessment flow
A linear, step-by-step flow reflects AN-ACC structure and reduces confusion.Evidence tagging
Staff can attach documents, notes, or observations directly to questions.Consistent hierarchy
Layouts were simplified to reduce cognitive load and improve scanning.Embedded progress notes
Users add context without leaving the workflow.Terminology alignment
Labels were updated to mirror language used in facilities.
Testing insights
Testing revealed clear expectations:
Users wanted reassurance about where they were in the flow
Evidence needed to be visible in context, not hidden
Navigation had to be predictable and stable
Terminology required refinement for clarity
Iterations implemented
Adding an editable progress note component
Refining the tagging workflow
Improving hierarchy to prevent navigation jumps
Updating terminology
Strengthening visual cues for progress
A structured assessment flow
Evidence tagging
Analysis of work delivered
Impact
Improved accuracy in AN-ACC preparation
Reduced anxiety for clerical staff
Consistent navigation and clearer hierarchy
Stronger evidence capture for audits
Readiness across 60,000+ residential beds
Reinforced Clinical Manager’s leadership position
90% ease-of-use rating
“The UX is really impressive!” - Scalabrini
My role
Senior UX Designer leading:
Discovery and research synthesis
Workflow and interaction design
Component architecture and foundational patterns
Prototyping and iteration
Alignment with BAs, engineering, and clinical SMEs
Translating complex rules into clear user flows
Key statistics
< 2 min evidence lookup
Reduced from 6–10 minutes
+38% confidence
Staff preparing AN-ACC assessments.
Half the navigation steps
Single assessment screen, down from 4–5 disconnected screens
Clear audit-ready assessment trail
All the evidence found in context
Completeness & accuracy
Fewer follow-up corrections across all five facilities.
Reflection
This project required clear prioritisation and disciplined decision-making. The accelerated timeline and legacy system constraints shaped every stage of the work. By grounding the workflow in user insight and AN-ACC structure, we delivered a safer, clearer assessment experience that prepared providers for the funding transition. The project reinforced the importance of designing for long-term system evolution while delivering meaningful value immediately.