Kyra PAS: Designing Australia’s first FHiR-native Hospital Patient Administration System
A scalable, mobile-enabled foundation for patient flow, interoperability, and hospital-wide coordination.
Why hospitals needed change
Context
Most PAS products in Australian hospitals were antiquated (20+ years old) and difficult to adapt. They were monolithic, siloed across departments and sites, hard to integrate, and often relied on outdated patterns not aligned with modern interoperability standards .
Staff compensated with paper, memory, or duplicate data entry, especially in the Emergency Department where speed and clarity matter most. These gaps created risk across patient safety, accuracy, and system interoperability.
Telstra Health set out to build a modern PAS from the ground up: FHIR native, mobile enabled, cloud hosted, and designed for single-instance deployments across multiple sites to remove fragmentation and standardise workflows.
Problem
Hospitals needed a system that supported:
Faster, safer ED administrative capture
Clear visibility of patient movement
Predictable workflows under pressure
Strong alignment with EMR, Bed Management, and downstream systems
A modular rollout (no “big bang” switch
Modern interoperability (FHIR, SNOMED CT, HL7)
Retrofitting the legacy PAS was unsafe. The structure and terminology of those products were too rigid, hard-coded, and incompatible with FHIR-aligned workflows.
Project Scope
Role
Lead UX Designer
Timeline
6 Months
Company
Telstra Health, Hospitals & Connected Health
Focus
Emergency Department admission pathway for the PAS MVP
Why legacy PAS workflows failed ED operations
Research and insights
Research included interviews with clerical staff, SME consultation, analysis of local PAS products, international review, and mapping of FHIR Patient, Encounter, and Location resources.
Six themes emerged:
Fear of errors
Staff worried their actions might cause downstream issues.Cognitive overload
Legacy screens were dense and spread across multiple locations.Paper reliance
Staff used paper to stabilise patient information quickly.Poor movement visibility
Whiteboards, spreadsheets, or memory were used to track positions.Terminology inconsistency
Every site used slightly different labels and processes.Integration gaps
Duplicate data entry across systems created risk and rework.
User frustrations presented with Fiorella, the administrator who wants a simple, intuitive and reliable workflow.
Recurring themes across clerical and clinical staff.
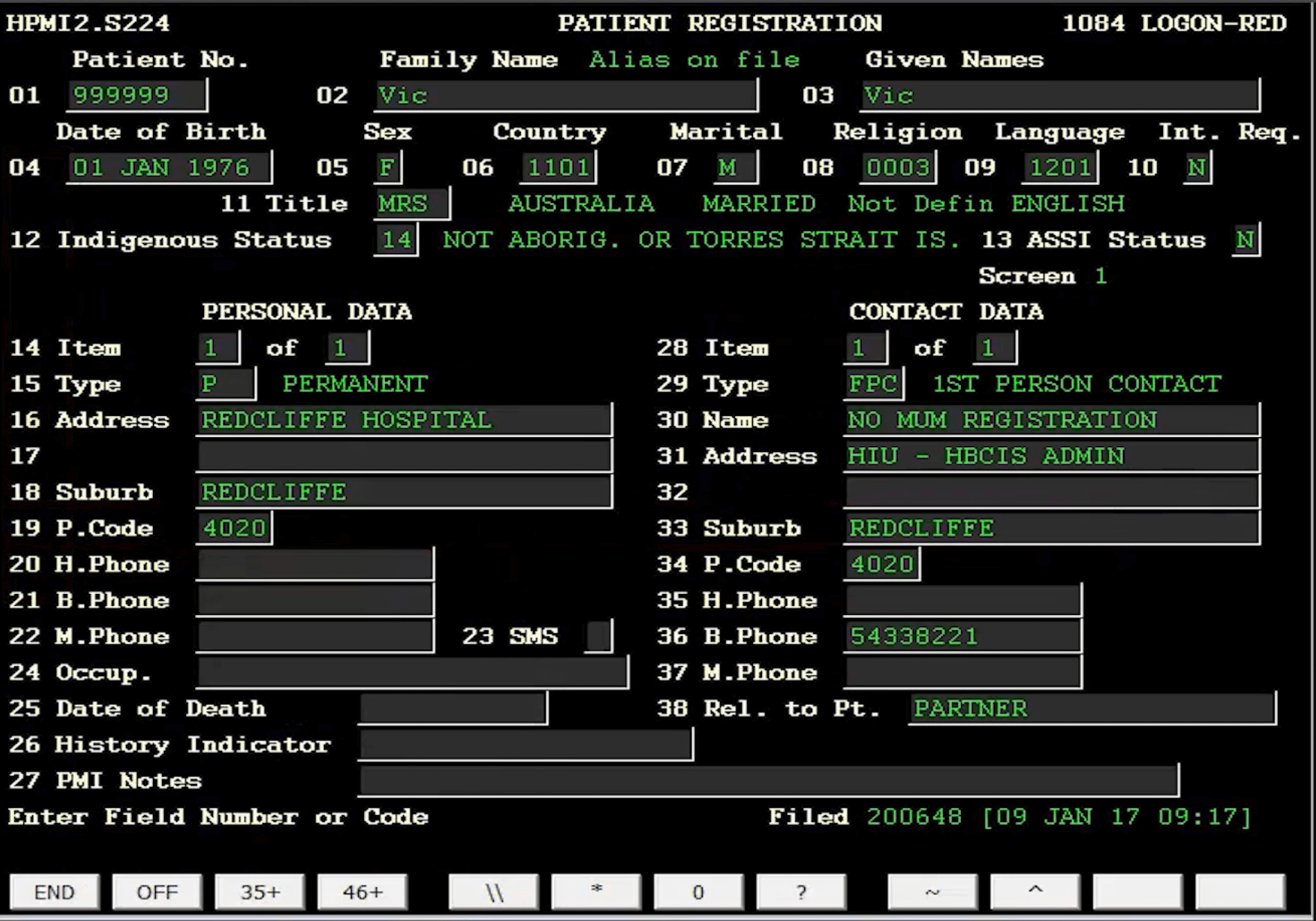
Above are two examples of current PAS used in Australian hospitals
What this meant for design
A new architecture and interface were essential.
Our PAS needed to deliver:
A safe and fast ED intake
Clear, real-time movement
Low cognitive load
Consistent terminology
Predictable, reversible actions
Accurate mapping to FHIR data structures
Defining the ED admission for MVP
Why the emergency dept came first
The Emergency Department is the hospital’s primary entry point. Errors or delays here create flow-on impacts across inpatient, theatre, and bed management operations. By focusing on ED, the team could demonstrate a safe architectural foundation without the risk of trying to cover the entire hospital at once.
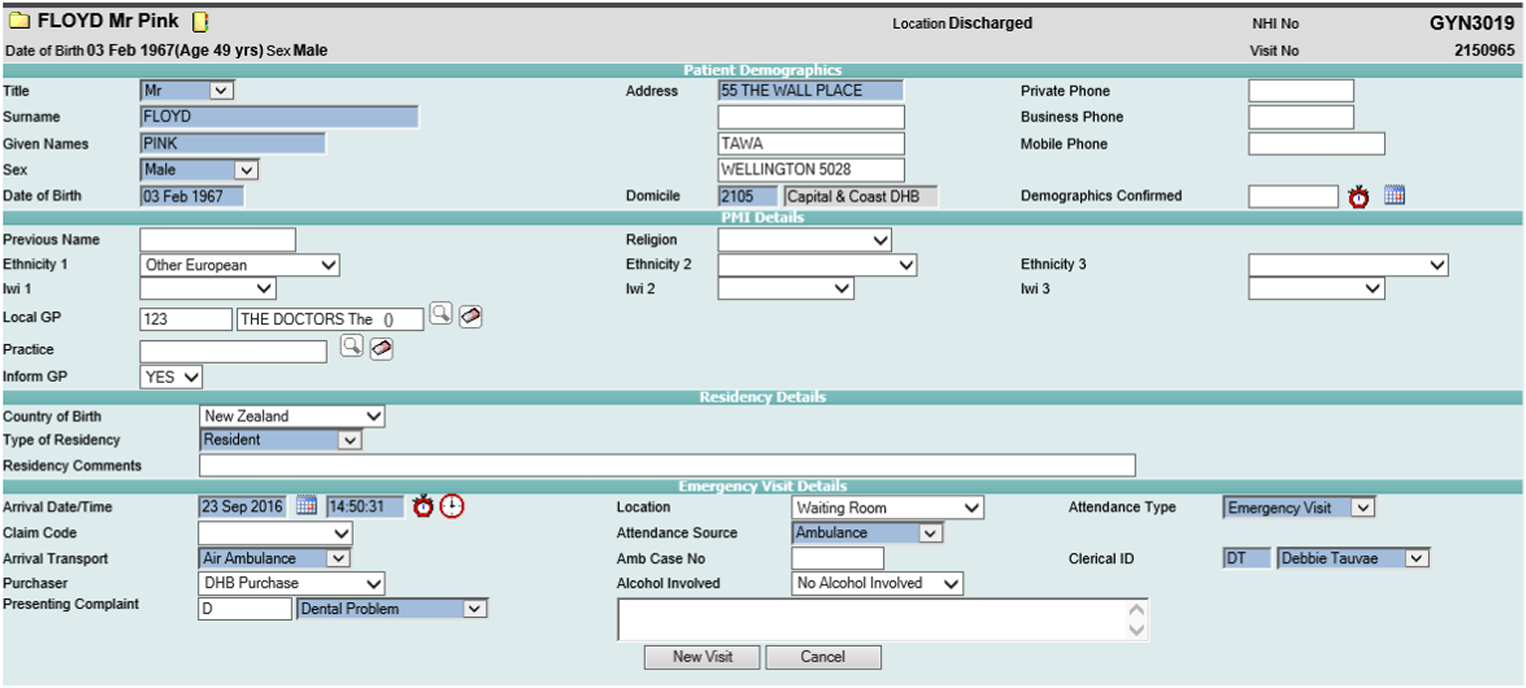
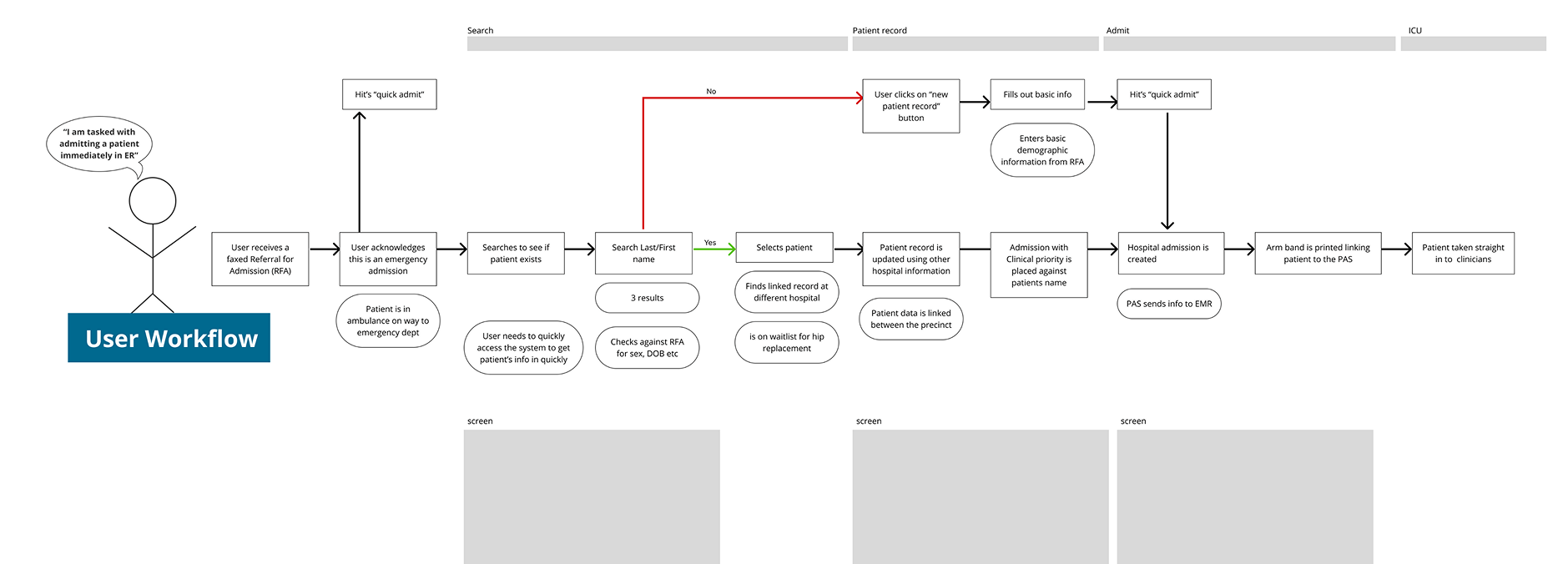
PAS user actions across the emergency department of a hospital.
The ED admission path
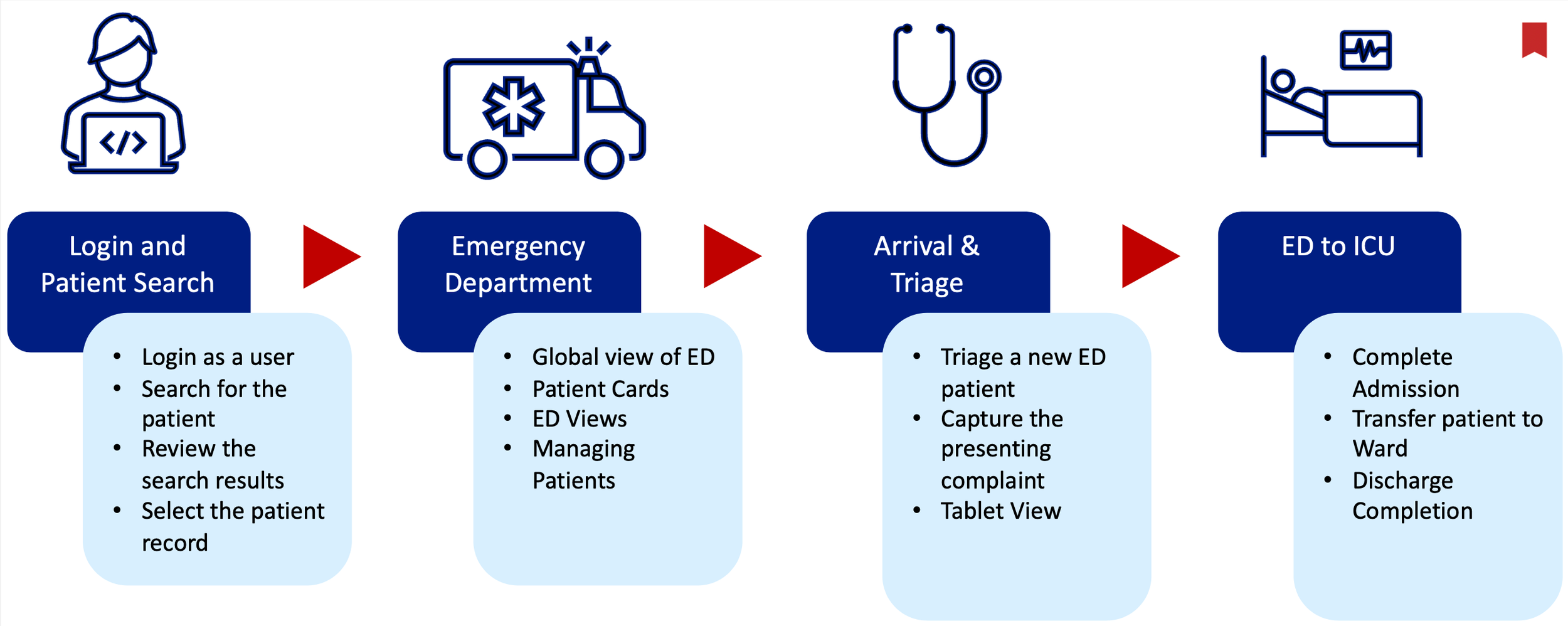
We modelled the admission process through the lens of Arthur (patient persona) and Fiorella (admin persona).
Critical path:
Referral received
Quick admit
Check or create patient
Print armband
Send encounter data to EMR
This sequence defined the essential screens and data objects needed to prove the PAS architecture.
Patient persona of Arthur, who we follow on his journey through the emergency department.
Mapping the ED admission process to identify PAS touchpoints and the foundational screens for MVP.
Architecture, strategy, and design
Strategic foundations
Kyra PAS is built on:
A single instance PAS model supporting multi-site organisations
A Clinical Data Repository (CDR) enabling staged migration from legacy PAS products (no risky big-bang implementation)
FHIR-native data structures for clean integration with EMR, Bed Management, Analytics, and Outpatients
Common terminologies (SNOMED CT) for semantic consistency across the hospital
Cloud hosting in Azure for lower infrastructure overhead and enterprise security
These architectural choices set a modern baseline for future hospital modules: Inpatients, Outpatients, Theatres, Maternity, Waitlist, and Billing.
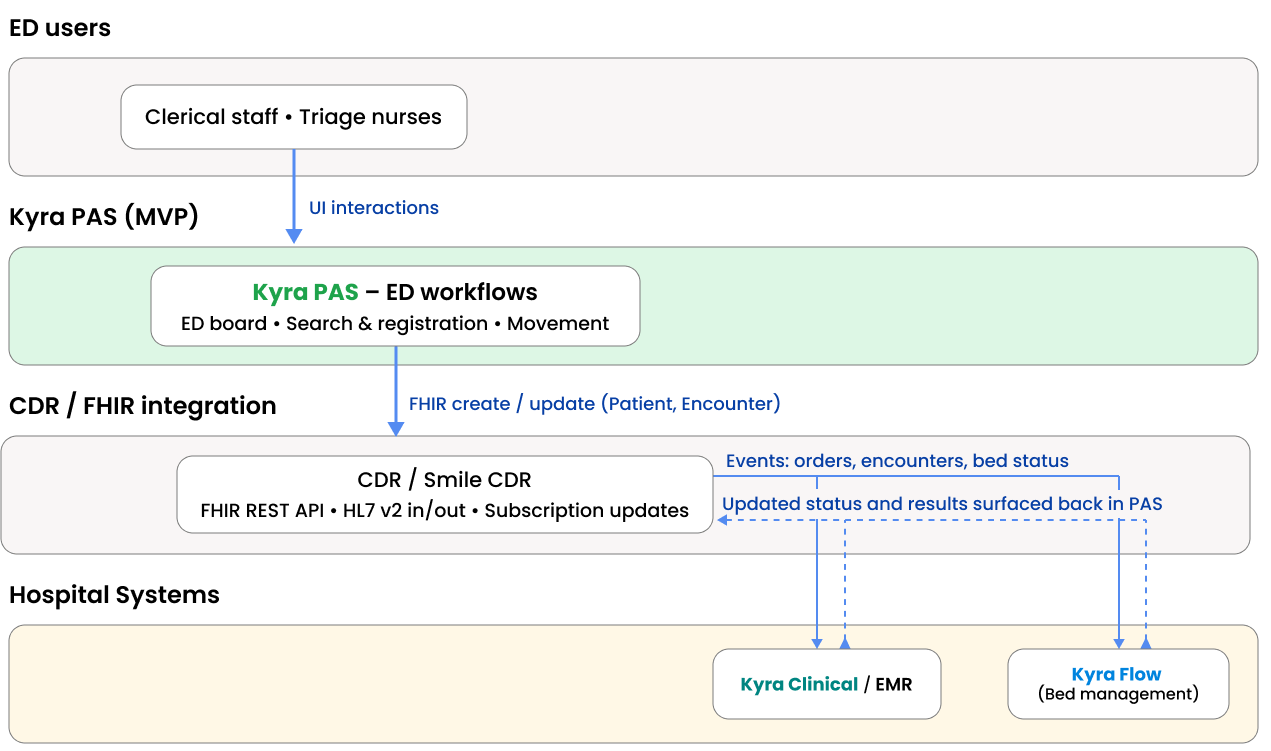
MVP Architecture:
ED users → Kyra PAS (ED workflows and screens) → FHIR via CDR → EMR and Bed Management → back to ED via updated status.
Architecture of MVP shows that Kyra PAS owns the ED workflows and screens, exchanging FHIR resources through the CDR and surfacing status from EMR and Bed Management back into the ED board.
Design strategy
Anchor the PAS around the ED workflow
Build a reusable patient card matched to FHIR resources
Create a single ED board for flow visibility
Keep interactions predictable and consistent
Reduce cognitive load through progressive disclosure
Mirror the mental model of ED teams
Produce a feasible MVP within six months
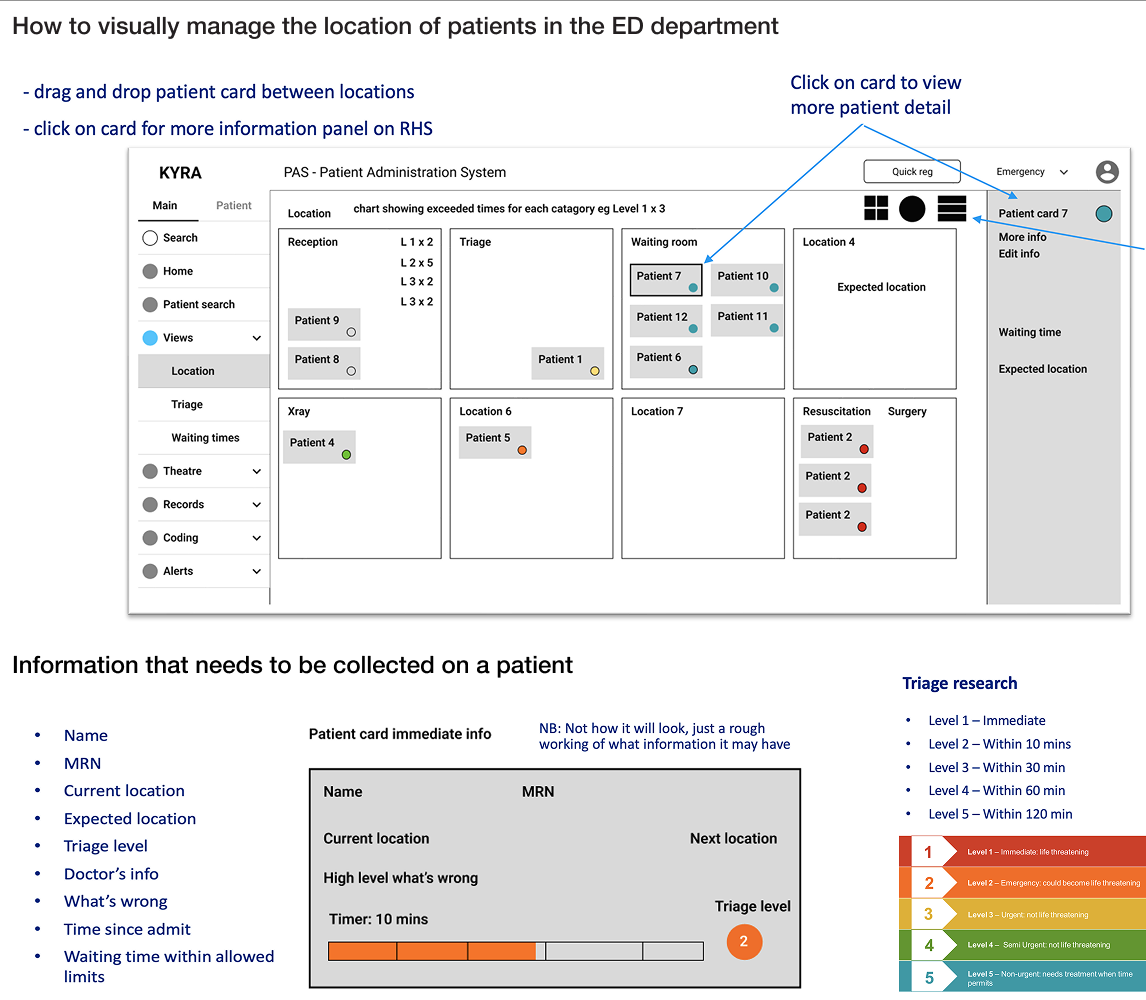
Wireframe of the PAS showing high level information that needed to be included.
The resulting layout
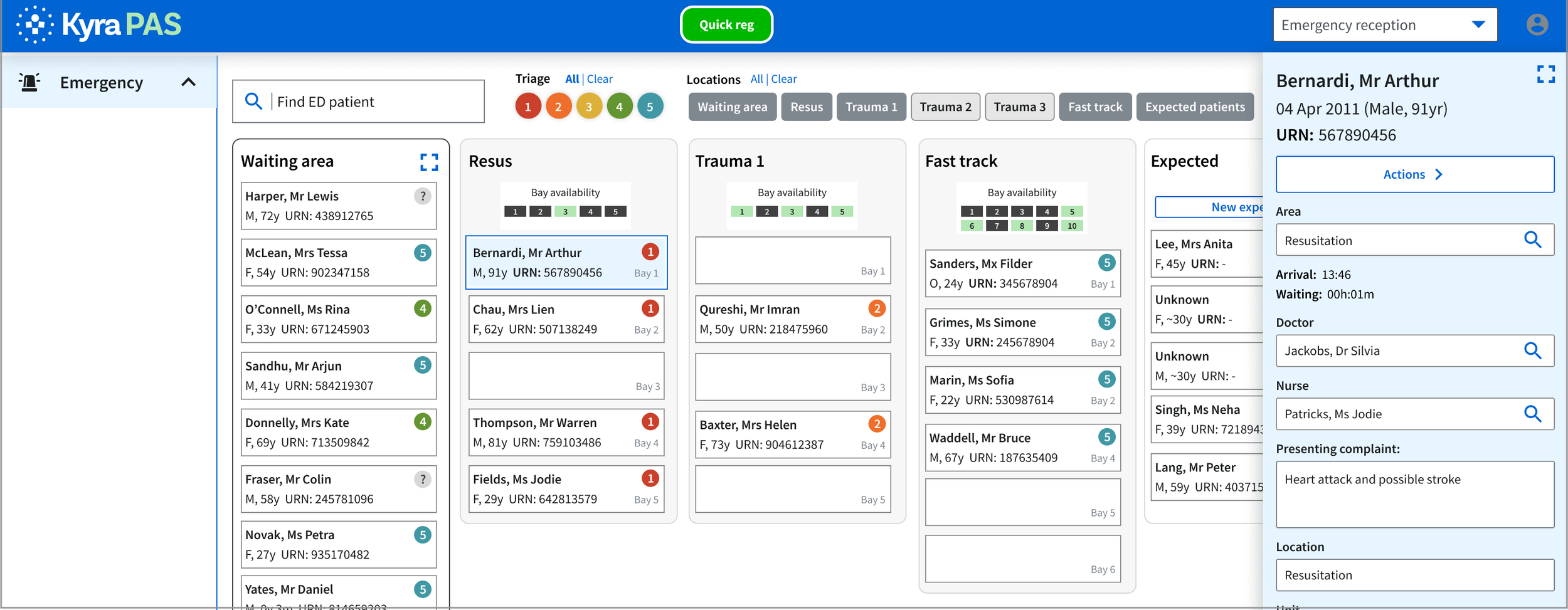
Designs moved away from the "ugly and confusing" legacy interfaces to a clean, block-based layout.
Location board: A grid view representing physical hospital locations (Triage, X-ray, Surgery).
Quick actions: A persistent "Quick Admit" button to handle emergency intake without navigating away from the board.
Bed availability indicators: Within locations a visual representation of available beds.
Patient overview: Selecting a patient card, a slide out drawer with high level editable fields within easy access.
Emergency Department board showing live patient flow, location capacity, and a slide-out patient summary for rapid updates.
Key design decisions
| Decision | Explanation |
|---|---|
| Structured arrival flow | Captured essential data early, delaying non-critical details to reduce load. |
| Reusable patient card | Modelled on FHIR Patient + Encounter. Supported consistent views across modules. |
| ED movement board | Provided a single high-value surface for tracking patient flow. |
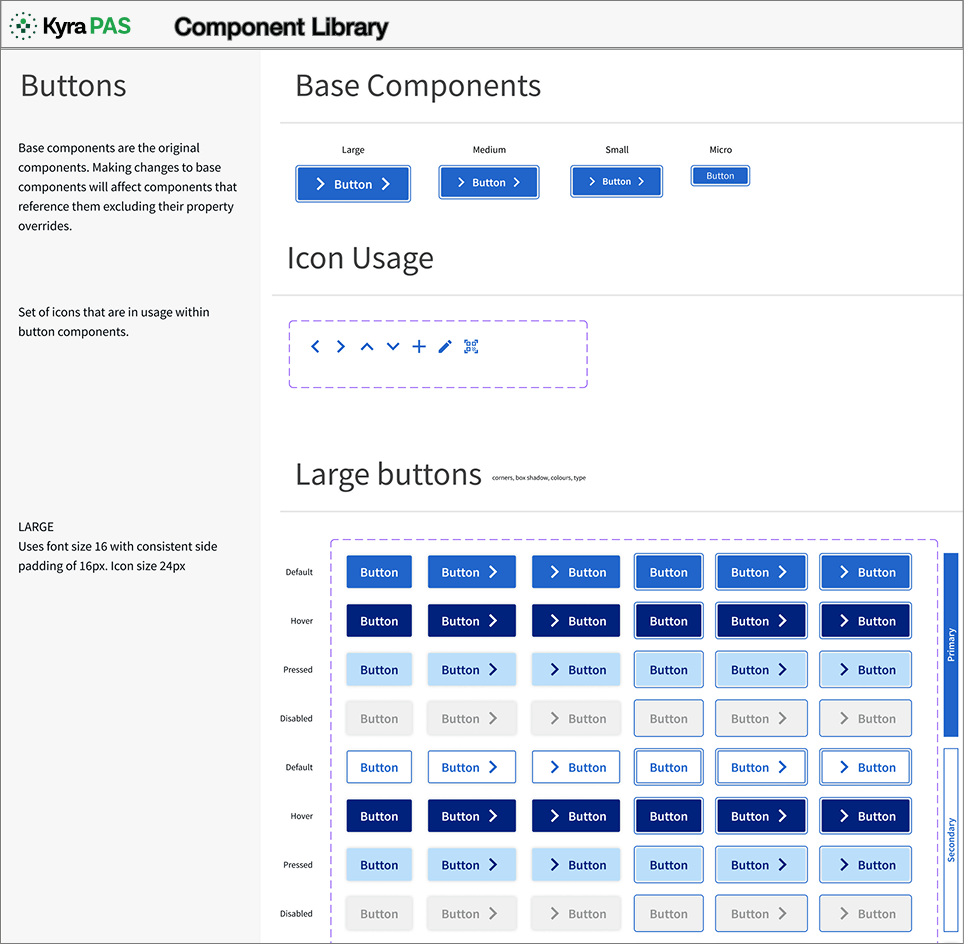
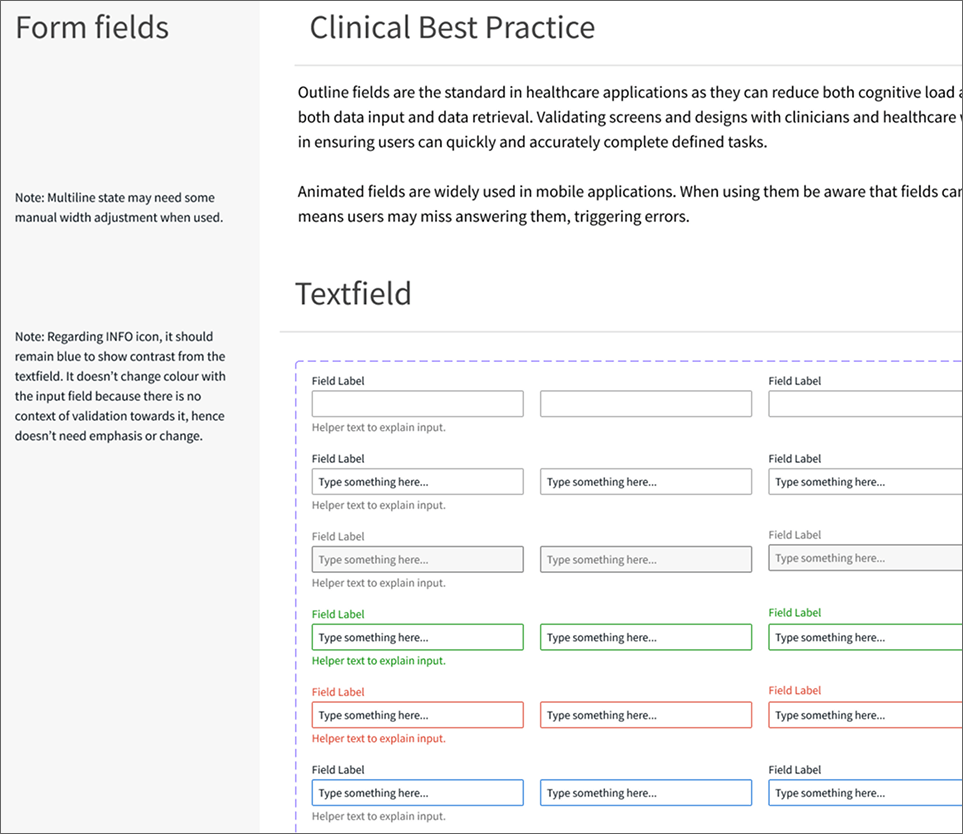
| Component library | Accelerated delivery and ensured consistent UI as modules expanded. |
| Terminology alignment | Ensured the interface matched real-world language. |
| Status + timer indicators | Quick risk identification for exceeded triage wait times. |
Component library examples showing buttons and form fields with alternate status states and consistent icon usage for healthcare workflows.
Testing, iteration, and refinement
Validation
Testing included SME walkthroughs, engineering feasibility checks, flow alignment with architect, and iterative prototyping.
Remote walkthrough session with clinicians and the delivery team during the validation phase.
What testing revealed
Clinicians needed clearer section delineation to maintain situational awareness.
Movement cues required stronger signalling during scroll and collapse events.
Navigation patterns needed consistency at both entry and exit points of the workflow.
Field grouping and sequence influenced registration accuracy and throughput.
Terminology and mandatory fields required configuration for local clinical practice.
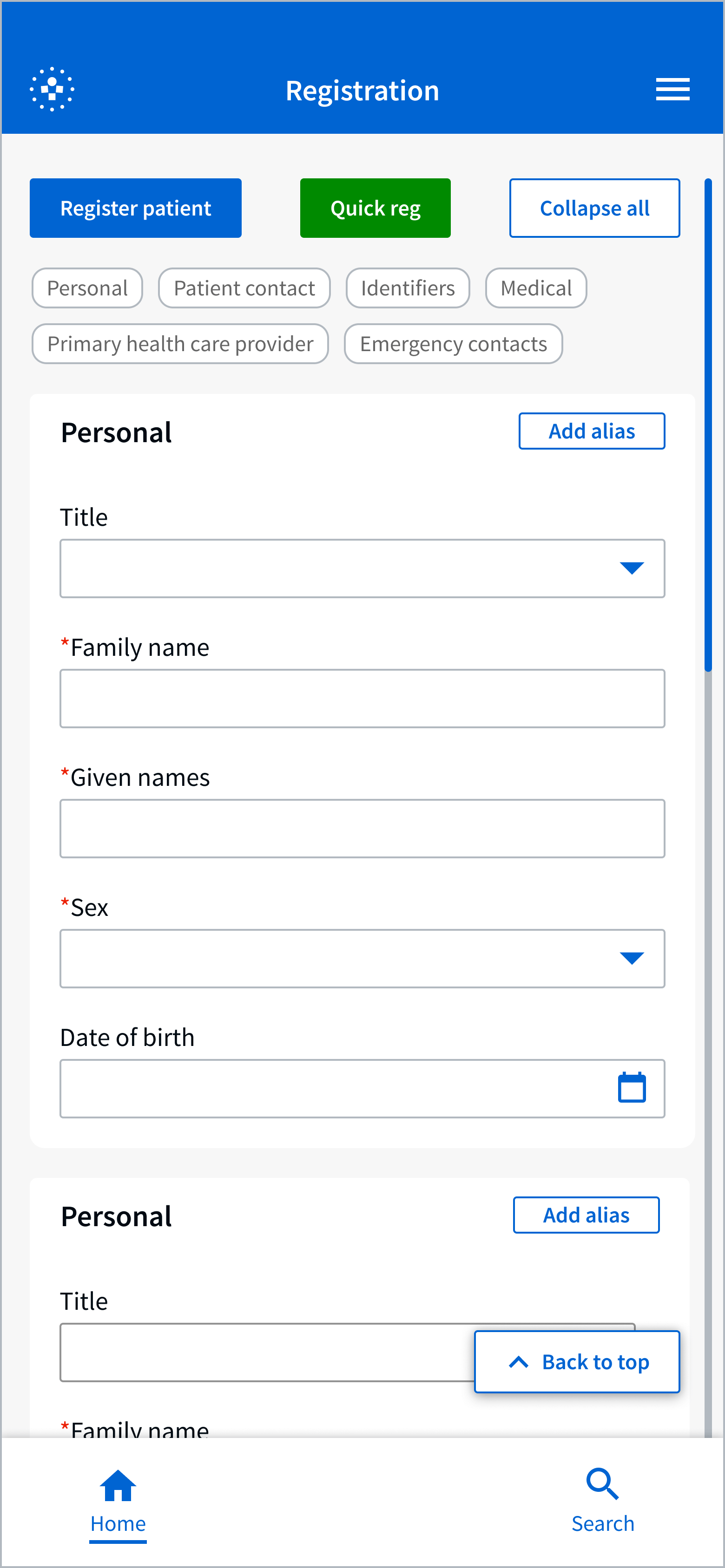
Mobile registration flow used in testing. Sessions showed users struggled with long-scroll fields, unclear section boundaries and inconsistent navigation states, which informed refinements to grouping, hierarchy and status indicators.
Key iterations
Strengthened hierarchy and section dividers.
Added persistent navigation patterns.
Refined field grouping for faster completion.
Reduced visual noise across form states.
Enhanced visibility of required data elements.
Achieving the outcome
How we achieved our aims
We met the goal of designing a modern PAS architecture by:
Delivering a FHIR-native MVP that proved the data model
Creating a reusable component library for future modules
Replacing fragmented screens with a single ED board
Using the CDR to support safe migration from legacy PAS products
Aligning all workflows with real clinical and clerical needs
Structuring ED movement into a clear, intuitive UI
Preparing the system for multi-site, multi-module scalability
These advances directly align with Telstra Health’s positioning of Kyra PAS as a single-instance PAS, designed to eliminate siloed workflows and create a consistent user experience across all hospital locations .
National launch showcasing Kyra PAS as a central component of Telstra Health’s next generation health platform.
Launch and stakeholder response
Kyra PAS was introduced at a national launch event that brought together senior clinical, operational and digital health leaders. The showcase positioned PAS as a core component of Telstra Health’s broader Kyra ecosystem and highlighted how a modern, standards-aligned platform supports safer and more connected care.
The response from stakeholders reflected strong sector alignment.
Clear demand for a contemporary PAS designed around real clinical workflows.
Recognition of the improved ED flow and reduced cognitive burden.
Validation of the modular, FHIR-aligned architecture for future expansion.
Interest from health services exploring progressive adoption across sites.
Early conversations on integration pathways and transition planning.
Reflections
My role
As the sole designer I delivered:
Research synthesis
ED workflows and UI design
Component architecture
Prototypes for all ED scenarios
Alignment with stakeholders, engineering, and SMEs
MVP scope shaping and risk reduction
Iteration cycles and decision facilitation
Our first team session in the Adelaide office
Reflection
The compressed timeline and limited access to frontline ED staff required disciplined prioritisation and fast, well-reasoned decisions. Focusing on the ED workflow helped clarify what mattered most and ensured the team delivered a coherent, testable MVP.
Centering the design around clear patterns, reusable components and a stable hierarchy improved the experience for users working under pressure. The work also showed that a modern, interoperable PAS is achievable when technical and design decisions stay tightly aligned.
Kyra PAS now offers a strong base for future modules and extensions, setting a clearer direction for how hospital administration systems can evolve.