Redefining Emergency Department patient administration using a FHIR-native model
Legacy Patient Administration Systems slow hospital operations and break down under Emergency Department conditions.
Linear workflows, heavy data requirements, and tightly coupled integrations push staff to paper workarounds and delayed reconciliation. This work defined a new PAS model designed to support uncertainty, handover, and time-critical admissions while integrating cleanly with modern hospital platforms.
At a glance
Delivery focus: Proof-of-life PAS MVP for Emergency Department admissions
System shift: FHIR-native PAS operating alongside EMR and patient flow systems
Scope: Admission workflows under emergency, time-critical conditions
Operating environment
Context
Organisation: Telstra Health
Environment: Hospital administration and patient flow systems
Users: Emergency Department administrative and clinical staff
Role: Lead UX Designer
Timeframe: 6-month MVP delivery
Constraints
Coexistence with legacy PAS
Complex integrations and reporting dependencies
Clinical safety and data integrity requirements
No external user testing budget
What existed and why it mattered
PART 1
The outcome
At the end of six months, the work resulted in:
a working PAS MVP covering a complete Emergency Department admission journey
a coherent interaction and system model aligned to FHIR data structures
a demonstrable product showing how PAS could operate alongside EMR and patient flow systems
a clear technical and product direction suitable for continuation and expansion
This phase was not intended to demonstrate adoption or efficiency gains. Success was defined as viability, coherence, and technical credibility.
Why PAS breaks down in Emergency
Emergency Departments operate with:
uncertain or partial patient identity at arrival
frequent interruptions and handovers
rapid movement across physical locations
high cognitive load and time pressure
Most legacy PAS platforms assume:
complete data capture upfront
linear task completion
single-system ownership of patient information
These assumptions do not hold in ED.
In practice, staff rely on paper, memory, or duplicate entry to stabilise patient flow. PAS interaction is deferred until workload allows, and records are corrected later. This behaviour is not accidental. It is a response to systems that slow care when used as designed.
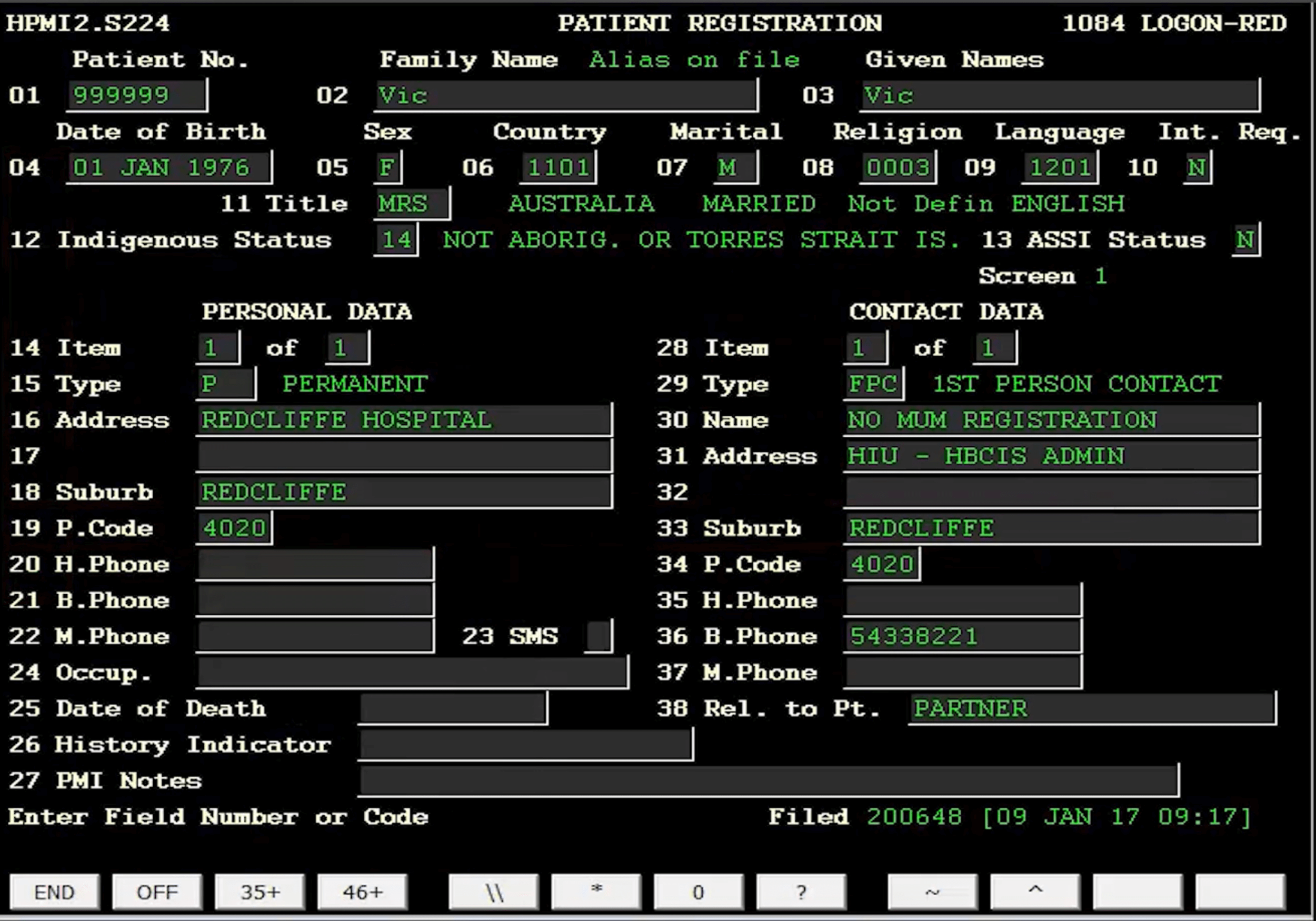
Visual 1 - Legacy PAS reality. PAS interfaces being used in Australian hospitals . These prioritise exhaustive data entry over flow, creating cognitive load and error risk under pressure.
Duplication and multi-system fragmentation
Hospitals operate multiple systems that capture overlapping patient information:
Patient Administration Systems
Electronic Medical Records
Bed management and patient flow tools
Department-specific systems
These systems often store similar data using different identifiers, formats, and update rules. When identity or encounter data cannot be safely amended in real time, duplication becomes the default.
Multiple records are created for the same patient and reconciled later.
This duplication increases:
downstream error risk
administrative rework
reporting inconsistencies
loss of confidence in the system of record
PAS failure in ED is therefore not a UI problem. It is a system integrity problem.
Why this problem persisted
PAS sits at the centre of hospital operations and underpins:
funding and reporting
billing and compliance
clinical and operational workflows
hundreds of system integrations
Most PAS platforms are:
over twenty years old
monolithic and tightly coupled
heavily customised per site
risky to change incrementally
Retrofitting legacy PAS introduces safety and governance concerns. As a result, many organisations avoid change entirely. Innovation stalled, and workarounds became normalised.
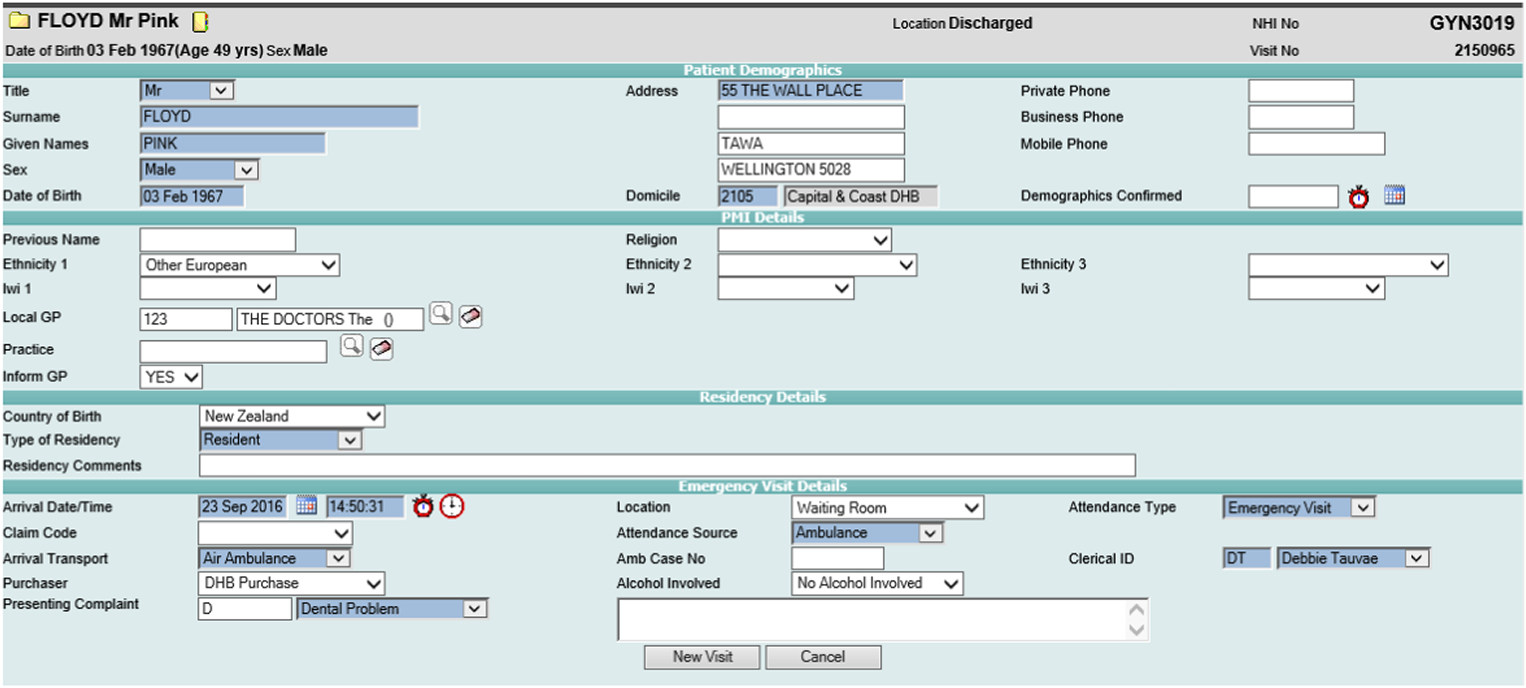
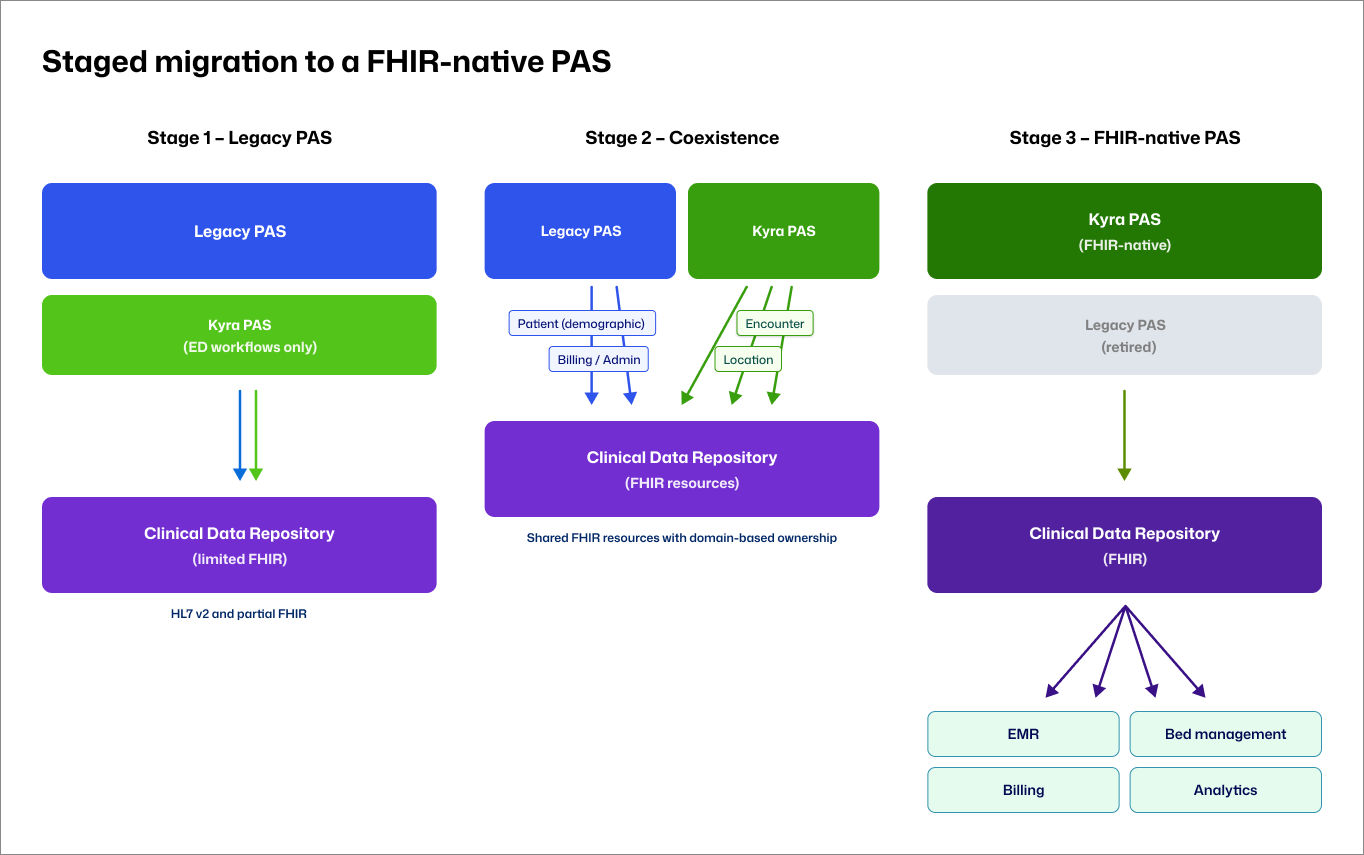
Why a FHIR-native model changes PAS behaviour
FHIR is a modern healthcare data standard designed to support interoperability between systems.
Rather than treating patient data as something owned by a single system, FHIR enables a distributed model where multiple systems participate in maintaining a shared view of patient information.
What FHIR enables
Patient, Encounter, and Location as discrete resources
Core concepts are modelled independently and linked, rather than embedded in a single record.Incremental updates instead of transactional overwrites
Information can be added or refined over time without requiring full record completion upfront.Correction and versioning without losing history
Data can be amended safely while preserving an audit trail.Multiple systems reading and writing to the same data layer
PAS, EMR, patient flow, billing, and analytics systems can interact with shared data without duplicating records.
Why this mattered for PAS
Traditional PAS platforms assume ownership of the patient record and enforce completeness early in the workflow. This clashes with Emergency Department reality, where information is often partial and evolves over time.
A FHIR-native PAS does not need to own the full record. Instead, it can:
support uncertainty and staged data capture
allow patient identity to be refined as information becomes available
coexist with legacy PAS during transition
reduce duplication by design rather than policy
This shifts PAS from a monolithic system of record to a collaborative participant in a broader hospital data ecosystem.
Visual 2 - FHIR-native PAS system model The PAS participates in a shared clinical data layer rather than acting as a siloed system of record.
Insight
A FHIR-native PAS shifts from record ownership to participation in a shared clinical data ecosystem.
Designing a viable PAS system for Emergency
PART 2
Framing the work as system validation, not feature design
This phase focused on validating whether a modern PAS model could operate safely within real Emergency Department conditions.
The objective was not to design a complete PAS. It was to demonstrate that a new system model, interaction approach, and data architecture could support a critical hospital workflow without relying on legacy assumptions.
The work treated Emergency admission as a system problem spanning people, software, data, and governance, rather than a sequence of screens.
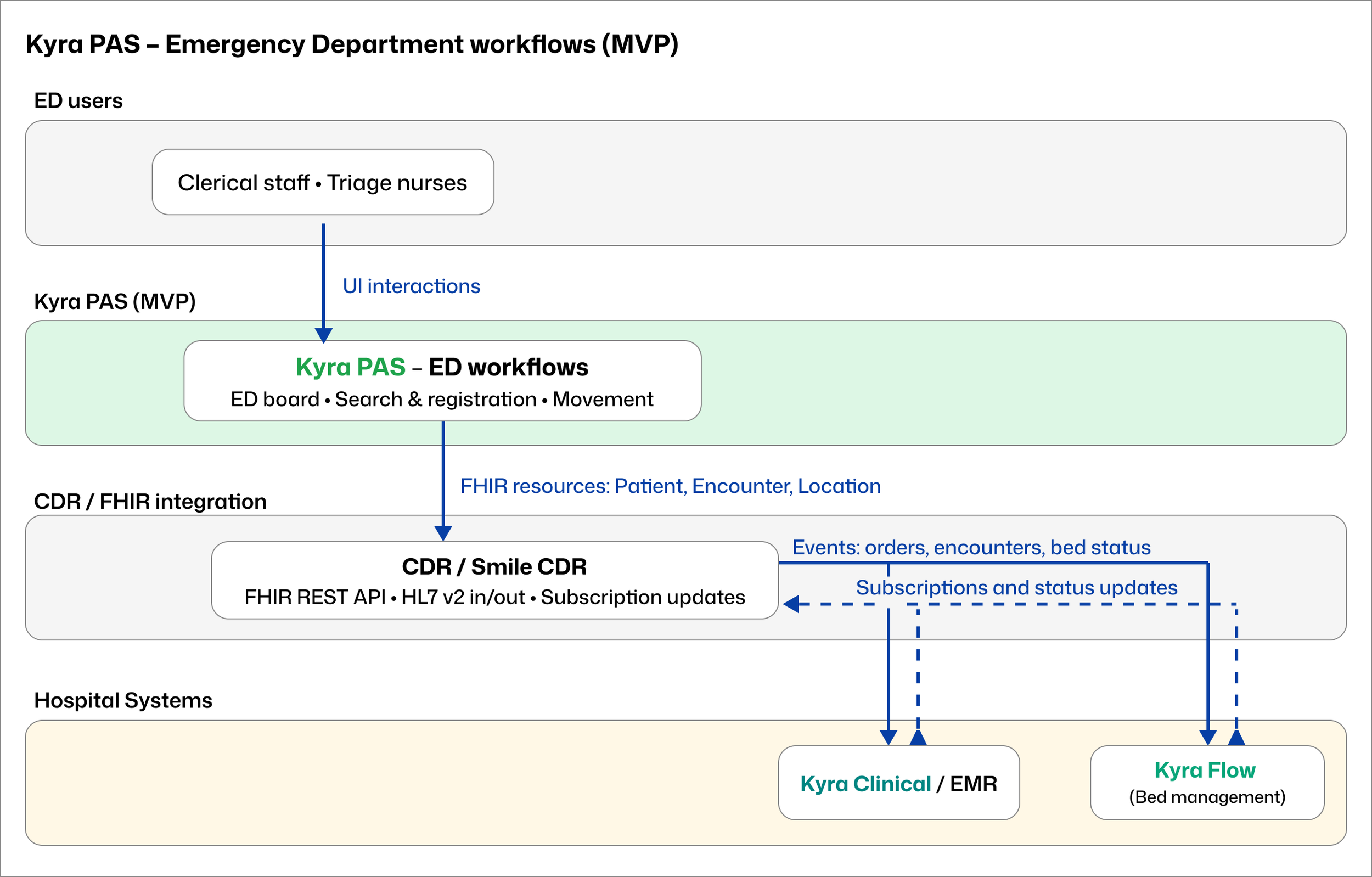
Defining the MVP patient journey
The MVP was deliberately scoped to a single, high-risk journey:
ED arrival and triage
Identity check or creation
Patient movement across ED locations
Admission completion
Transfer out of ED
This journey represented the minimum path required to validate the PAS model.
If ED admission could operate safely under time pressure, uncertainty, and handover, the underlying architecture and interaction patterns could scale to the rest of the hospital.
Visual 3 - ED MVP journey map Shows how Kyra PAS supports safe progression from arrival to transfer when identity is partial, time is constrained, and patient location changes frequently.
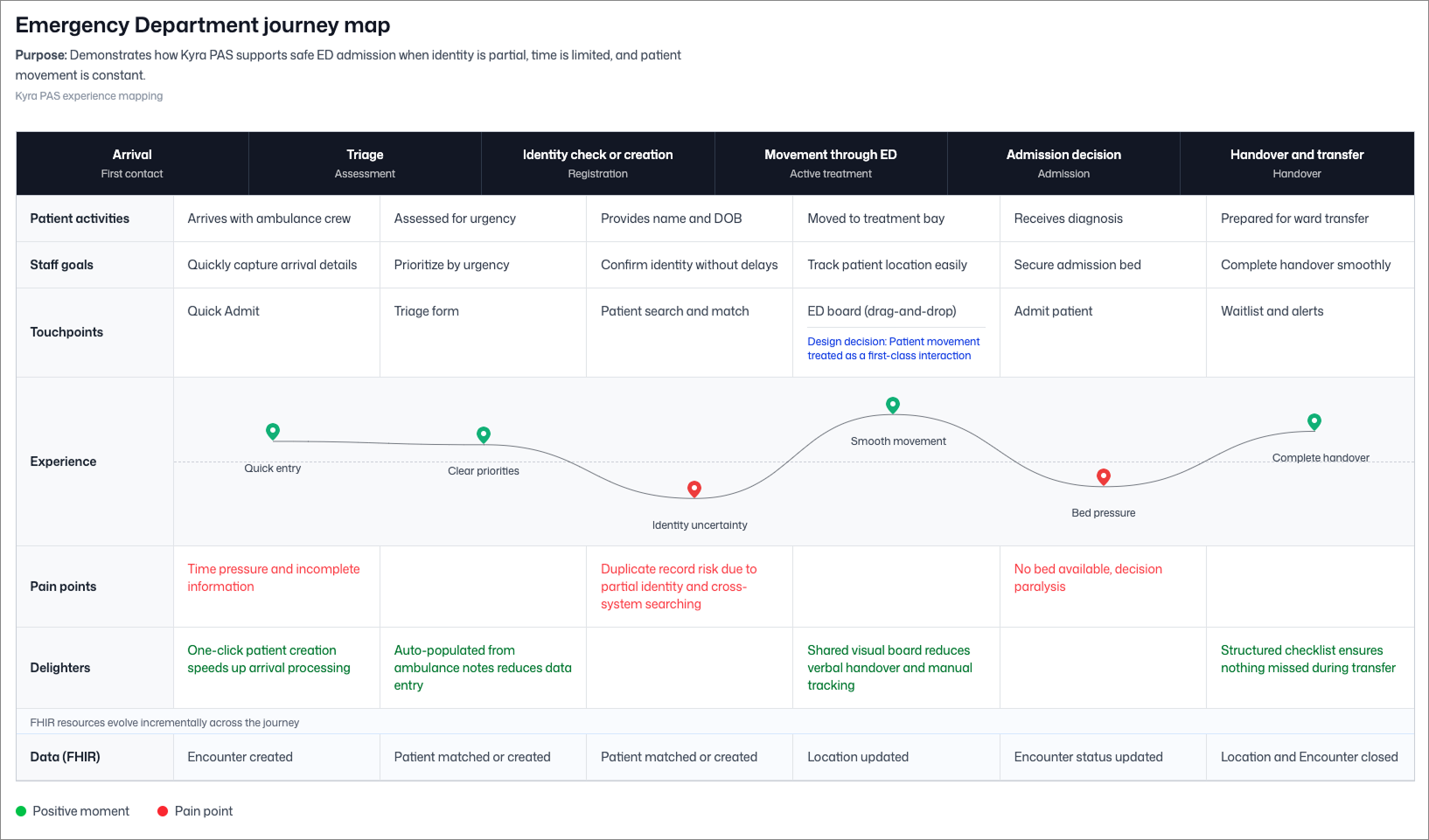
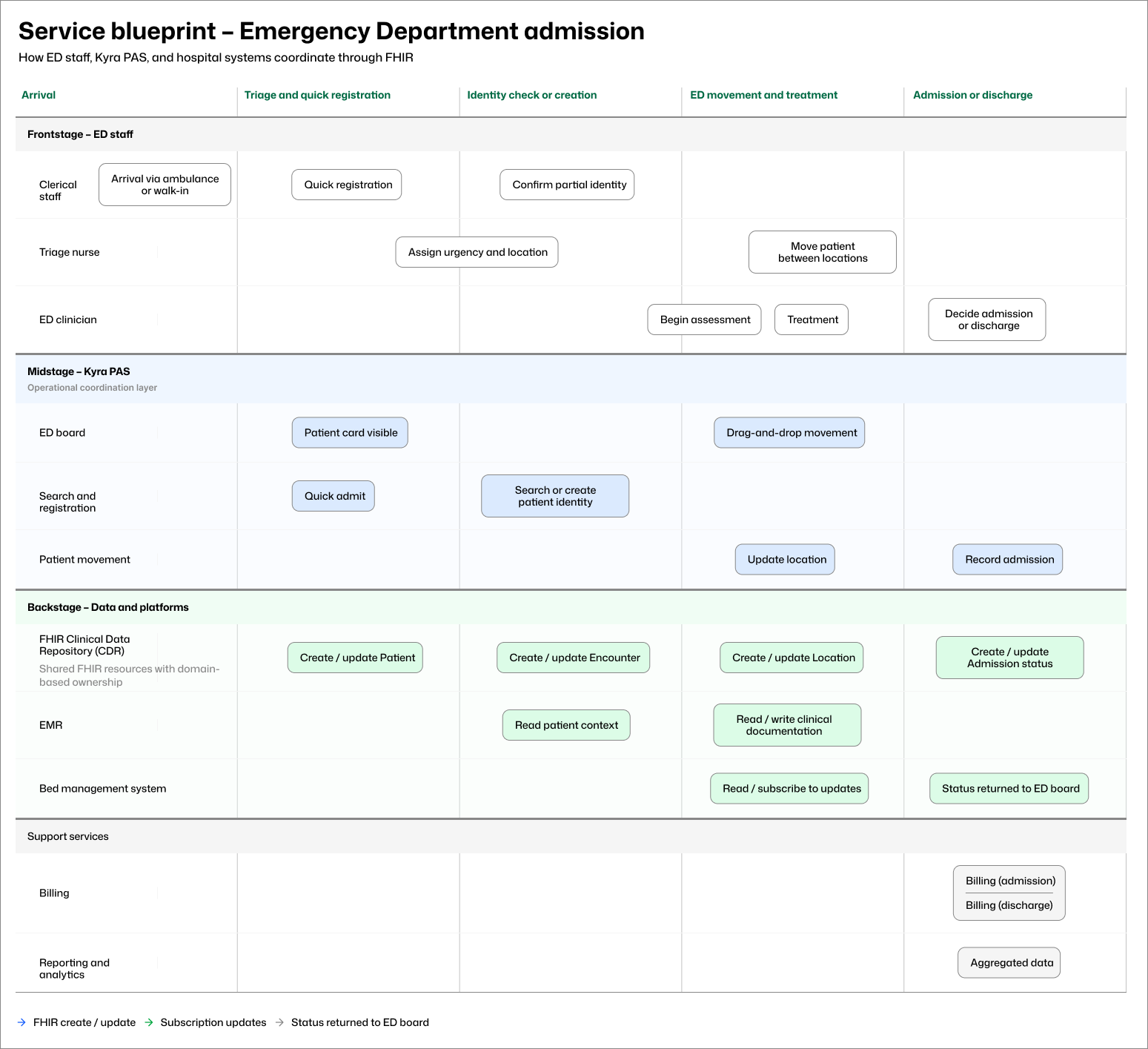
Coordinating people, product, and data
Emergency admission involves:
frontstage activity by clerical staff, triage nurses, and clinicians
midstage coordination through the PAS
backstage data updates across EMR, bed management, billing, and reporting systems
Rather than treating these as separate concerns, the work mapped them together to ensure interaction design, system behaviour, and data ownership remained aligned.
Creating the service blueprint clarified:
where uncertainty enters the workflow
which system owns which decisions at each stage
how FHIR resources are created and updated incrementally
how downstream systems remain informed without blocking ED flow
This artefact makes explicit how admission work, system behaviour, and data responsibilities align across roles and systems.
Visual 4 - Service design blueprint. Shows how ED staff, Kyra PAS, the FHIR Clinical Data Repository, EMR, bed management, and downstream services coordinate during Emergency Department admission.
Designing without a built system or testing budget
There was no production system and no budget for external user testing.
Validation relied on:
Low-fidelity wireframes reviewed with engineering
SME walkthroughs with nurses, doctors, and PAS specialists
Architectural alignment sessions
Frequent internal critique and iteration
Design progressed from structural wireframes to interaction models, then to working prototypes suitable for demonstration.
Decisions were validated through coherence across the service blueprint, interaction flows, and data model.
Designing for real ED pressure
The design strategy prioritised:
predictable interaction patterns
reduced cognitive load
clear visibility of patient state and movement
minimal disruption during interruptions and handover
Key decisions included:
anchoring the PAS around the ED workflow
consolidating flow visibility into a single operational surface
maintaining consistent navigation across screens
limiting cognitive load through progressive disclosure
aligning terminology with real-world clinical practice
The work prioritised clarity and predictability for staff operating under sustained time pressure and frequent interruption.
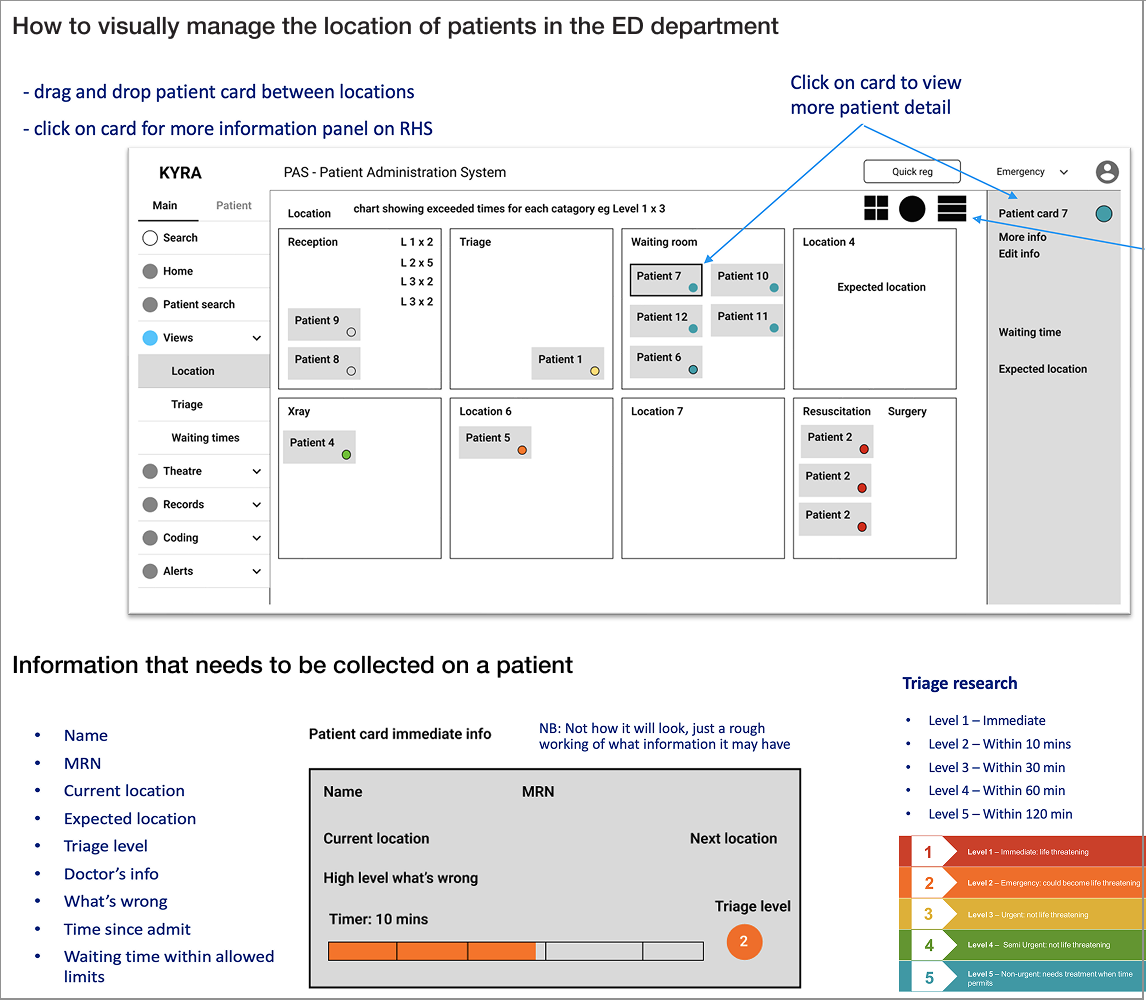
Patient movement as interaction
A major departure from legacy PAS was treating patient movement as a primary interaction rather than an administrative task.
Instead of navigating multiple screens or forms:
Patients move visually between locations
State updates automatically
Timers and status indicators remain visible
Detailed actions are accessible without breaking flow
This supported rapid situational awareness during high-pressure moments.
Visual 5 – Working prototype Showing ED movement and search
Decision
Patient movement was treated as a first-class interaction to support situational awareness under pressure.
Concrete design decisions
This interaction model required a small set of explicit, repeatable design decisions.
Design decisions were explicit and repeatable:
a reusable patient card mapped to FHIR resources
a central ED movement board as the primary surface
consistent arrival and admission flows
component-based UI for scalability
terminology alignment to reduce ambiguity
status and timer indicators to support triage awareness
Validating interaction before visual refinement
Visual 6 – Interaction wireframes Interaction wireframes used to define triage logic, patient cards, and detail panels underpinning the working prototype. Focus was placed on flow, sequencing, and safety-critical information rather than visual refinement.
Working without clinical training
As the sole designer without a medical background:
Product experts, nurses, and doctors were consulted frequently
Assumptions were validated through discussion rather than preference
Language, sequencing, and edge cases were pressure-tested
Decisions were grounded in operational reality
This reinforced a workflow-first, system-led design approach rather than an interface-led one.
Results, measurement and impact
PART 3
How success was measured
Success criteria were defined for a proof-of-life phase.
Primary measures
a complete ED admission journey could be demonstrated end-to-end
identity uncertainty could be handled without blocking flow
data structures aligned to FHIR and supported correction over time
the system story held together technically and operationally
Quantifiable indicators available at this stage included:
six-month delivery of a working MVP
number of core workflows demonstrated live
breadth of system integrations shown in architecture artefacts
scale of stakeholder engagement during showcase sessions
Demonstration and reception
Kyra PAS was presented broadly across the health portfolio.
attendance exceeded 400 stakeholders
feedback focused on feasibility and clarity of direction
discussion centred on next steps rather than fundamental viability
Visual 7 - MVP showcase milestone Shows Kyra PAS presented as a viable platform direction to a broad health leadership audience.
Outcome
Stakeholder discussion shifted from viability to continuation and scale.
Technical credibility
The demonstration showed:
FHIR-based data exchange
coexistence with legacy PAS
HL7 v2 integration paths
SMART on FHIR extensibility
Visual 8 - Staged migration to a FHIR-native PAS Illustrates how Kyra PAS enables staged migration rather than wholesale replacement of legacy PAS.
Reflection and next steps
What this work established
a viable PAS interaction model
a defensible technical foundation
a clear demonstration of PAS operation under real hospital conditions
This was foundational work rather than a polished product.
Limits of the timeframe
Six months constrained:
depth of functionality
external validation
breadth of scenarios
Next steps identified
extend the MVP to additional admission scenarios
deepen identity and duplicate-management tooling
formalise a PAS design system
validate workflows in live hospital environments